Phlebolymphedema
UNDERSTANDING PHLEBOLYMPHEDEMA: CAUSES, SYMPTOMS, AND MANAGEMENT
Phlebolymphedema is a complex condition that affects millions worldwide, yet it often goes unrecognized or misunderstood. This article aims to shed light on this challenging disorder, providing valuable information for both the general public and those living with the condition.
What is Phlebolymphedema?
Phlebolymphedema is a chronic condition that results from a combination of venous insufficiency (problems with blood flow in the veins) and lymphedema (swelling due to a buildup of lymph fluid). It typically affects the lower limbs, causing persistent swelling, discomfort, and potential complications if left untreated.
Causes and Risk Factors
Understanding the root causes of phlebolymphedema is crucial for both prevention and management. The condition arises from a complex interplay of factors:
1. Venous Insufficiency: When veins in the legs fail to efficiently return blood to the heart, it can lead to fluid accumulation.
2. Lymphatic System Dysfunction: If the lymphatic system is compromised, it struggles to drain excess fluid from tissues.
3. Obesity: Excess weight puts additional pressure on both the venous and lymphatic systems.
4. Sedentary Lifestyle: Lack of movement can impair circulation and lymph flow.
5. Genetics: Some individuals may have a genetic predisposition to venous or lymphatic disorders.
6. Previous Injuries or Surgeries: Trauma to the legs or lymph nodes can increase the risk.
Did you know? Recent studies suggest that up to 5% of the global population may be affected by some form of chronic edema, with phlebolymphedema being a significant subset of this group.
Symptoms and Diagnosis
Recognizing the signs of phlebolymphedema is the first step towards proper management. Common symptoms include:
• Persistent swelling in the legs or feet
• Feeling of heaviness or tightness in the affected limb
• Skin changes, including thickening or hardening.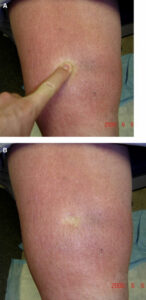
• Reduced range of motion
• Recurrent infections in the affected area
Diagnosis typically involves a combination of:
7. Physical Examination: A healthcare provider will assess the affected area and review medical history.
8. Imaging Tests: Ultrasounds or MRIs may be used to evaluate blood flow and lymphatic function.
9. Bioimpedance Analysis: This test measures fluid levels in body tissues.
Early diagnosis is crucial for effective management. If you experience persistent swelling or any of the above symptoms, don’t hesitate to consult a healthcare professional.
Treatment Options
While there’s no cure for phlebolymphedema, various treatment options can significantly improve symptoms and quality of life:
10. Compression Therapy:
• Custom-fitted compression garments or bandages
• Pneumatic compression devices for home use
11. Manual Lymphatic Drainage:
• Specialized massage techniques to stimulate lymph flow.
• Often performed by certified lymphedema therapists
12. Exercise and Movement:
• Tailored exercise programs to improve circulation.
• Aquatic therapy can be particularly beneficial.
13. Skincare:
• Meticulous skin hygiene to prevent infections.
• Use of moisturizers to maintain skin health
14. Weight Management:
• Maintaining a healthy weight can significantly reduce symptoms.
15. Medications:
• Diuretics may be prescribed in some cases.
• Antibiotics for treating or preventing infections.
16. Surgical Interventions:
• In severe cases, procedures like lymph node transfer or liposuction may be considered.
Treatment Success Rates: Studies have shown that comprehensive treatment programs can lead to significant improvement in over 70% of patients with phlebolymphedema.
Living with Phlebolymphedema
Managing phlebolymphedema is an ongoing process, but with the right approach, individuals can lead fulfilling lives:
17. Adherence to Treatment: Consistency is key in managing symptoms effectively.
18. Self-Care Routines: Develop daily habits for skin care and gentle exercises.
19. Emotional Support: Connect with support groups or counseling services to address the psychological impact.
20. Lifestyle Modifications:
• Elevate legs when resting.
• Avoid prolonged standing or sitting.
• Wear loose-fitting, comfortable clothing.
21. Regular Follow-ups: Maintain ongoing communication with your healthcare team.
22. Stay Informed: Keep up to date with the latest research and treatment options.
Quality of Life Impact: Recent studies indicate that proper management can lead to a 40-60% improvement in quality-of-life scores for individuals with phlebolymphedema.
Conclusion
Phlebolymphedema is a challenging condition, but with proper understanding and management, its impact on daily life can be significantly reduced. If you suspect you may have phlebolymphedema, don’t hesitate to seek medical advice. Remember, early intervention and consistent management are key to maintaining your health and quality of life.
Living with phlebolymphedema may seem daunting, but you’re not alone. With the right support and treatment plan, you can take control of your health and lead a fulfilling life. Stay informed, stay positive, and most importantly, stay proactive in your care.

